Osteoporosis: A Deeper Dive
Osteoporosis: A Deeper Dive, provides an overview of the disease, with scientific and medical expressions explained in simple terms.
What is osteoporosis?
Osteoporosis, meaning “porous bone”, is a bone disorder that causes decreased bone strength and density. This can lead to an increased risk of fracture.
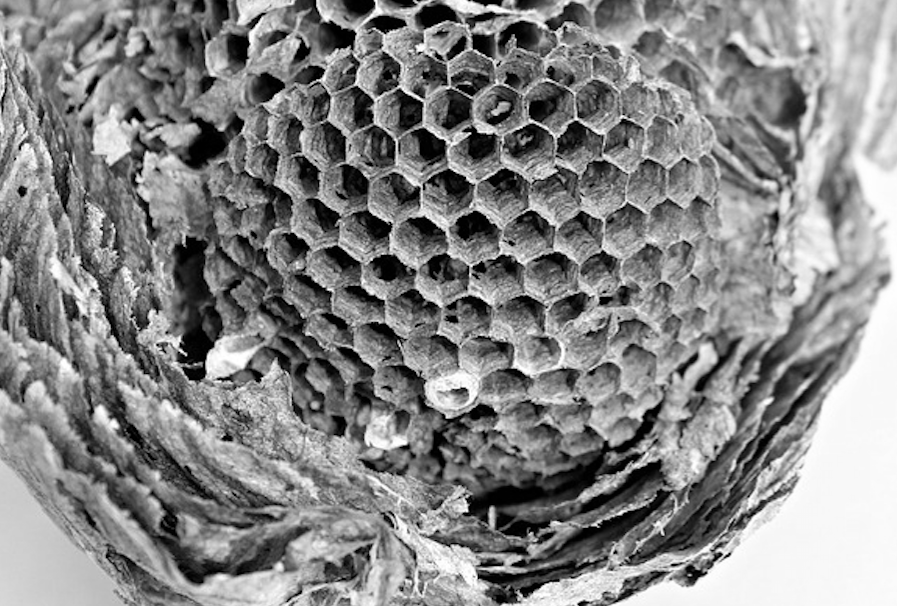
Bones have a smooth outside surface, but the inside is structured like honeycomb. This honeycomb mesh structure gives bones their strength, but when osteoporosis sets in the honeycomb starts to break down, creating patches within the bone that are unsupported. This means that the smooth outside layer is all that’s holding the bone together, and with the slightest knock it can break apart.
In a little more detail: bones are at their most dense between the ages of 20 and 30. After that, the cells in the bone that have been constantly renewing, change from building bone to breaking bone down. This breaking down of the bone is called catabolism. The resulting loss of bone mass happens mainly on the endosteal surface, which is the inner surface of the smooth bone, and in trabecular bone, which is the honeycomb structure.
How do bones work?
The skeletal bones found in the ground and used as flame-bearing torches in Indiana Jones movies, are hard. But while your body lives the osseous tissue, the strong connective tissue that forms your bones, is far less rigid and far more changeable. This is because bone is in an ever evolving state, made from a mixture of:
- Collagen proteins that provide flexibility
- Hydroxyapatite, a bone mineral containing calcium and phosphate that gives bones their characteristic rigidity and strength
Cells called osteoclasts and osteoblasts repair and modify bones as the body ages. In simple terms, osteoclasts consume bone while osteoblasts build bone. This means that bones are in a constant state of change, adapting to the stresses and strains they’re put through.
Peak bone mass, achieved between the ages of 20 and 30, depends on genetic factors along with contributions from:
- Nutrition
- Endocrine status – the hormonal balance that maintains consistent bodily function. Imbalances are often associated with women, but can affect people of any age and any gender
- Physical activity
- Health during growth
A brief history of osteoporosis
1824 – Osteoporosis was first codified as a disease in its own right and considered an unavoidable aspect of ageing.
1882 – German doctors considered it a ‘woman’s condition’, with breaks caused by tripping over their long skirts.
1903 – Article published in The New Zealand Observer and Free Lance described the condition as something contagious and primarily affecting horses.
1930s – U.S. endocrinologist Fuller Albright linked the disease to hormones and specifically to menopause. This discovery led it to be reframed as a disease, and therefore treatable, rather than just part of the ageing process.
2008 – Introduction of the trabecular bone score (TBS), which allowed for measurement of the microarchitectural structure of bone tissue.
What causes osteoporosis?
Too little formation of bone, or too much removal of bone by osteoclasts, occurs as a result of external factors, either genetic or environmental.
It’s most often caused by decreased oestrogen. Oestrogen is a hormone that controls the number of osteoclasts. When oestrogen levels fall, osteoclasts multiply and more bone gets broken down.
Unchecked osteoclasts break-down bone at a faster rate than osteoblasts can rebuild. This leads to a progressive weakening of the bone.
It is estimated that 80% of osteoporosis cases occur in women, however osteoporosis has been under-diagnosed and under-treated in men, leading many to think that it’s far more common in men than has previously been thought. It is estimated that 50% of caucasian women will experience an osteoporotic fracture in their lifetime, and 20% of men.
For women, oestrogen levels dip significantly after menopause, which is why it’s almost expected that women will get osteoporosis at some point. But after the age of 30, male oestrogen levels also fall consistently by 1% every year. This means that male osteoporotic fractures tend to occur between 5 and 10 years later than in women.
Along with the natural hormonal alterations that occur through age, there are certain medical conditions or lifestyle choices that can cause osteoporosis at an earlier age.
Lifestyle factors:
- Alcohol abuse
- Smoking – active or passive
- Frequent falling – often through contact sports
- Lack of exercise
- Vitamin D insufficiency
- Excessive thinness – often caused by eating disorders
- High salt intake
- Low calcium intake
- Excess of vitamin A
- Lack of mobility – caused by certain medical conditions
Genetic diseases:
- Cystic fibrosis
- Glycogen storage diseases
- Hypophosphatasia
- Parental history of hip fracture
Gastrointestinal disorders:
- Celiac disease
- IBD (inflammatory bowel disease)
- Primary biliary cirrhosis
- Gastric bypass
- Gastrointestinal surgery
- Pancreatic disease
Rheumatologic and autoimmune diseases:
- Ankylosing spondylitis
- Rheumatoid arthritis
- Other rheumatic and autoimmune diseases
Neurological and musculoskeletal:
- Epilepsy
- Parkinson’s disease
- Multiple sclerosis
- Spinal cord injury
- Muscular dystrophy
- Stroke
Other conditions and diseases:
- AIDS/HIV
- Chronic obstructive lung disease
- Congestive heart failure
- Chronic metabolic acidosis
- Depression
Medications:
- Aromatase inhibitors
- Depo-medroxyprogesterone (premenopausal contraceptive)
- Tamoxifen (premenopausal use)
- Anticoagulants
- Barbiturates
- Glucocorticoids
- Methotrexate
- Some serotonin inhibitors
- Chemotherapy drugs
- Anticonvulsants
- Excessive thyroid hormones
The signs and symptoms
The problem with osteoporosis is that there are none. Often called “the silent disease”, weakening bones isn’t something that’s felt, it’s something that becomes apparent after it’s already manifested and the first fracture occurs. Fractures can be caused by mild traumas, or in extreme cases spontaneously, with no trauma at all.
Recovery from fractures can be long, and some never fully regain mobility, especially if the fracture occurs in old age. The reason for this is simple; if the bone has been, and still is being, weakened by unchecked osteoclasts (cells that break down bone), then the osteoblasts (cells that rebuild bone) are already failing to maintain bone density, let alone being able to rebuild bone that is broken.
It is therefore much better to have an early and full assessment, as osteoporosis can be prevented if caught in the early stages of the disease.
If you are caring for someone with osteoporosis, the HomeTouch team can help. We can provide you with advice and support, and help you to find a top quality carer in your local area.
Just call 020 7148 0746.
The diagnosis
The King Faisal Specialist Hospital Osteoporosis Working Group recommends screening for women 65 years and older and for men 70 years and older. If a person is in a genetic risk group, or shows evidence of osteoporosis or has a disease that often leads to osteoporosis, they should also be screened.
In addition, any fracture that happens during adulthood may indicate the presence of osteoporosis, especially if the fracture occurs after only a minor trauma.
The National Osteoporosis Foundation recommends a comprehensive approach to the diagnosis, involving:
- A detailed history of the patient
- A physical examination
- A BMD (bone mineral density) assessment
- Vertebral imaging
Low BMD can be caused by hyperparathyroidism or osteomalacia, and these diseases have specific therapies, so it’s important that a BMD assessment is not the only test carried out.
T-scores and Z-scores
Are statistical numbers which factor in variables such as age, race, gender and presence of fracture. T-scores compare BMD to a young adult of the same sex. Z-scores compare BMD to a healthy person of the same age, sex and ethnicity. For this reason, Z-scores are becoming the more trusted reference.
- A normal T-score is -1.0 and above (normal bone density)
- A person with a T-score of -2.5 and below is likely to have osteoporosis
- A person with a Z-score of -2.0 or below is classified as having “low BMD for chronological age”
DEXA (DXA) scan: “dual energy X-ray”
A DEXA scan is a bone density scan and is used to diagnose or assess the risk of osteoporosis. The scan measures how much radiation passes through the bones. These numbers are compared to healthy bones in a young adult or a healthy adult of the same age.
Vertebral imaging
One fracture in the spine increases the risk of more fractures in the spine by 5-times, and the risk of other fractures by 2 to 3 times. A lateral thoracic and lumbar spine X-ray or lateral vertebral fracture assessment (VFA) are available on most DEXA machines and they can often be performed at the same time.
Other bone density tests
Some of the evaluations that laboratory assessments that test the underlying causes of osteoporosis are not as effective for men.
Some of the BMD screening technologies used for both men and women are:
CT-based absorptiometry: Quantitative computed tomography (QCT)
Measures volumetric integral, trabecular, and cortical bone density and can be used to determine bone strength. Within the bone, tissue forms a honeycomb structure. When osteoporosis occurs, the honeycomb structure becomes incomplete, leading to weakness. The QCT (and TBS) reveals how complete the bone structure is.
Trabecular Bone Score (TBS)
A technique of measuring the microarchitectural structure (honeycomb) of bone tissue.
Quantitative ultrasound densitometry (QUS)
This method doesn’t directly measure BMD, instead it measures speed of sound. If bones are dense, sound travels slower, revealing the health of bones. This method uses no radiation.
The treatments
The first treatment step is to treat the fracture. After this, treatment can be introduced to minimise the risk of further fractures.
Dietary preventions:
- Calcium
- Vitamin D
A balanced diet is rich in low-fat dairy products, fruits and vegetables, and provides the calcium and nutrients needed to maintain good health. If calcium levels can’t be maintained through diet, supplements can help.
Vitamin D plays a major role in calcium absorption, bone health and muscle performance, which also has an effect on risks of falling. Good sources of Vitamin D can be found in fortified milk and cereals, some fortified juices, salt water fish, and liver.
Exercise:
- Weight-bearing exercise
- Muscle strengthening exercise
Muscle strengthening exercise increases strength, agility, posture and balance, and reduces the risk of falls and fractures. This type of exercise includes:
- Weight training
- Yoga
- Pilates
Weight-bearing exercise means exercise where the bones and muscles work against gravity while the feet and legs bear the body’s weight. This type of exercise includes:
- Walking
- Jogging
- Tai Chi
- Stair climbing
- Dancing
- Tennis
Other:
- Quit smoking
- Get treatment for alcoholism, where necessary
Medications
Most osteoporosis medications either slow the breakdown of old bone, or speed the process of bone renewal. Some perform both functions. Long-term use of certain drugs can lead to side-effects, so your doctor may recommend a break from treatment after 3-5 years. The benefit of the medication will not stop during the ‘holiday period’, as the effects are long lasting.
Bisphosphonates
Can be taken in tablet form, as an injection, or through intravenous infusion (a drip). They’re generally well tolerated, although they can cause digestive problems if the instructions aren’t followed carefully.
Some less common side effects include itchy rashes, a sore mouth, flu symptoms, muscle pain, headaches.
Teriparatide and parathyroid
Parathyroid is a naturally occurring hormone that helps to regulate calcium levels. Teriparatide is a synthetic form of parathyroid. Both of these help with new bone formation, reducing the risk of future fractures.
These treatments tend to come in a pen-like syringe which can be used to self-inject. They’re usually prescribed for daily use for 18 months.
Some side-effects include palpitations, dizziness, headaches, fatigue, depression, and gastrointestinal problems.
Raloxifene
Is most often prescribed to postmenopausal women after a fracture. It has dual benefits, increasing bone density in the spine, and the risk of breast cancer. It’s taken in 60mg tablets once daily and some side effects include hot flushes, leg cramps, swollen ankles and flu-like symptoms.
Calcitonin
Is usually used as a short-term treatment immediately following a fracture, due to the fact that it prevents further bone loss. It is usually administered by injection, and some side effects include nausea, diarrhoea, flushing, dizziness.
Denosumab
Works by limiting the activity of the osteoclasts that destroy bone tissue. It’s taken by injection just twice a year, and side effects include back pain, UTIs, constipation and rash.
HRT (hormone replacement therapy)
Is often diagnosed as a short-term treatment for women who are experiencing menopausal symptoms. HRT helps to balance the sudden drop in oestrogen that can spark the beginning of osteoporosis. With these treatments there’s a small risk of breast and ovarian cancer, deep vein thrombosis, heart attack, stroke and memory impairment. However, it does reduce the risk of hip fracture and colon cancer.
The comorbidities
A comorbidity is a separate medical problem that is directly caused by an original disease or condition. The most common comorbidities are depression and anxiety, and as these can have a serious impact on quality of life, often leading to loss of interest in maintaining treatment regimes. For this reason it is very important that they are treated.
Because osteoporosis causes weakening of the bones, an osteoporotic fracture is likely to occur. The most common places to experience a fracture caused by osteoporosis are in the wrist, hip and spine. These fractures can result in:
- Severe, chronic pain
- Loss of height
- Stooped posture
- Restricted mobility
- Depression
Hip fractures are associated with an increase in mortality (likelihood of death) of between 8 and 36% for a year after the incident. Mortality rates are higher in men than in women. 20% of hip fracture patients require care in a nursing home, and on average only 40% regain their previous level of independence.
Spine fractures are painful, can cause disability, deformity and mortality. Multiple spine fractures can lead to lung disease and abnormal functioning of the abdomen, or stomach. This can lead to constipation, stomach pain and reduced appetite.
As fractures often cause pain, disability and changes to appearance, they can lead to depression, anxiety and loss of self-esteem.
How does osteoporosis affect normal life?
The effect of osteoporosis on life depends very much on how debilitating the condition is for the individual. For some, their condition barely impacts on their physicality, for others the results can be devastating.
After a severe fracture of the hip or pelvis it’s not unusual to require help with basic self-care, like using the bathroom and getting dressed. It’s not unusual for a person with osteoporosis to need help with cooking, cleaning and gardening, and measures should always be put in place to prevent further falls.
It is common for people with lasting osteoporosis in old age to require daily help from family, friends, or professional carers.
Caring for someone with osteoporosis
The key to helping someone with osteoporosis is to stay positive and be sensitive to their mental health and wellbeing. Pain isn’t fun, and managing a long-term condition can be draining. It’s important to adhere to medication and treatment regimens, and to keep-up with regular physical activity.
It is also important to take care of yourself. Caring for someone is rewarding, but it can also be incredibly challenging and stressful. Making sure you don’t neglect yourself can make a big difference to your own long-term health.
If you are caring for someone with Osteoporosis, HomeTouch can help. Simply search by postcode and browse the profiles of self-employed carers near you. All of the carers on our site have gone through a thorough 42-point vetting process, and only 5% are accepted. You choose the carer you want to work with, and we provide support with contracts, payments, and holiday and sickness cover.
Find out more:
- Where does osteoporosis start?
- Why osteoporosis is common in females
- What is the osteoporosis t-score?
Sources:
- National Rheumatoid Arthritis Society. Cimzia (certolizumab pegol). Available at: https://www.nras.org.uk/cimzia-certolizumab-pegol-. Last accessed 30/08/2017.
- NICE. Certolizumab pegol for treating rheumatoid arthritis after inadequate response to anti TNF inhibitor. Available at: https://www.nice.org.uk/guidance/ta415/chapter/1-Recommendations. Last accessed 31/08/2017.
- Montastruc J L et al. The discovery of vasomotor nerves. Clin Auton Res. 1996;6:183-187.
- https://link.springer.com/article/10.1007/BF02281906
- Endocrine Web. Researchers explain history of clinical concept of osteoporosis. Available at: https://www.endocrineweb.com/news/osteoporosis/6718-researchers-explain-history-clinical-concept-osteoporosis. Last accessed 29/09/2017.
- Kaufman JM et al. Treatment of osteoporosis in men. Bone. 2012. 53(1): 134-144. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3662207/
- Yu J. Endocrine disorders and the neurologic manifestations. Ann Pediatr Endocrinol Metab. 2014. 19(4): 184-190. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4316409/
- Chan JJ et al. QCT Volumetric bone mineral density and vascular and valvular calcification: the framingham study. J Bone Miner Res. 2015. 30(10): 1767-1774. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4809363/
- Cosman F et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporosis Int. 2014. 25: 2359-2381. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4176573/pdf/198_2014_Article_2794.pdf
- Compston J et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2017. 12(1): 43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5397452/
- Gillies GE et al. Estrogen action in the brain and the basis for differential action in men and women: a case for sex-specific medicines. Parmacol Rev. 2010. 62(2) 155-198. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2879914/
- Mic. Do men have estrogen? Yes, and it’s critical to their health. Available at: https://mic.com/articles/135096/do-men-have-estrogen-yes-and-it-s-critical-to-their-health#.Ehq1G6lrk. Last accessed 29/09/2017.
- Johns Hopkins Medicine. Metabolic bone disorders. Available at: https://www.hopkinsmedicine.org/metabolic_bone_center. Last accessed 29/09/2017.
- Arthritis Research UK. Drugs for osteoporosis. Available at: https://www.arthritisresearchuk.org/arthritis-information/drugs/drugs-for-osteoporosis.aspx. Last accessed 29/09/2017.
- Healthtalk.org. Impact on home life due to osteoporosis. Available at: https://www.healthtalk.org/peoples-experiences/bones-joints/osteoporosis/impact-home-life-due-osteoporosis. Last accessed 29/09/2017.