Alcohol-related dementia differs from other forms of dementia in one important way: with early clinical intervention and complete abstinence, cognitive function can often be stabilised and sometimes improved.
In this article, our clinical team explains what causes alcohol-related brain damage, the signs that indicate someone may need support, and the medical interventions that can help. If you’re concerned about a family member’s cognitive changes, this guide provides the clear information you need to take the next step.
Key insights
- Long-term alcohol use and vitamin B1 deficiency can cause alcohol-related dementia (ARD). Early treatment and abstinence may stabilise or improve symptoms.
- Recovery requires complete abstinence, medical supervision, nutritional support, and structured care.
- Specialist care at home helps maintain independence and provides clinical oversight throughout recovery.
Understanding alcohol-related dementia
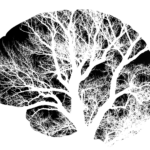
Prolonged alcohol use can damage brain cells, affecting memory, judgement, and behaviour. This is known as alcohol-related dementia (ARD), sometimes called alcohol-induced dementia or alcohol-related brain damage (ARBD).
Unlike most forms of dementia, alcohol-related dementia can be stabilised, and in some cases partially reversed, with early clinical intervention and complete abstinence from alcohol.
If you’ve noticed changes in a family member’s thinking, mood, or personality, our clinical team can help you understand what’s happening and what support is available.
What causes alcohol-related dementia?
Alcohol damages the brain through several mechanisms. It reduces blood flow and oxygen to brain cells, causing gradual shrinkage of certain areas – particularly the frontal lobes, which control planning, organisation, and emotional regulation. Over years of heavy drinking, this damage accumulates.
Vitamin B1 (thiamine) deficiency also plays a crucial role. Many people who drink heavily have inadequate diets, and a lack of thiamine causes further brain injury, worsening cognitive decline. Together, alcohol toxicity and vitamin deficiency create a damaging cycle.
The risk increases with:
- Heavy drinking over many years
- Repeated episodes of binge drinking
- Poor nutrition or vitamin B1 deficiency
- Head injury, liver disease, or compromised general health
How alcohol-related dementia differs from Alzheimer’s disease
Alcohol-related dementia and Alzheimer’s disease share some symptoms (such as memory loss and confusion), but they have different underlying causes. Alzheimer’s is a neurodegenerative condition involving abnormal protein buildup in the brain, whereas alcohol-related dementia results from toxic and nutritional damage.
Unlike Alzheimer’s disease, alcohol-related dementia can improve if the person stops drinking and receives appropriate medical treatment. However, if drinking continues, symptoms progress rapidly.
Other forms of alcohol-related brain damage
Wernicke-Korsakoff syndrome
This is the most severe form of alcohol-related brain damage and results from vitamin B1 deficiency.
- Wernicke’s encephalopathy is the acute stage. Symptoms appear quickly and include confusion, loss of balance, eye movement problems, and difficulty walking. This is a medical emergency requiring immediate treatment with thiamine injections.
- Korsakoff’s syndrome often follows Wernicke’s encephalopathy. It causes severe short-term memory loss and confabulation, when someone unintentionally creates stories to fill memory gaps. With alcohol abstinence and proper nutrition, some recovery is possible.
Frontal lobe damage
Heavy drinking can shrink the frontal lobes, which manage reasoning, self-control, and emotional response. People may appear apathetic, impulsive, or socially inappropriate. This form of ARD is sometimes called frontal lobe dementia.
Vascular damage
Alcohol can raise blood pressure and damage blood vessels, increasing the risk of small strokes and vascular dementia. While vascular dementia itself is irreversible, stopping alcohol use can prevent further damage.
Common signs and symptoms
Each person experiences alcohol-related dementia differently, but common symptoms include:
- Increasing confusion or forgetfulness
- Difficulty planning, organising, or problem-solving
- Poor judgment or decision-making
- Loss of motivation and initiative
- Personality or mood changes, such as irritability or apathy
- Impaired balance or coordination, even when sober
- Emotional outbursts or unpredictable behaviour
- Difficulty maintaining relationships
Unlike Alzheimer’s disease, many people living with alcohol-related dementia retain skills and knowledge learned in childhood. However, recent memories and daily routines often become confused.
Diagnosis and when to seek help
If you suspect alcohol-related dementia, speak to a GP as soon as possible. Doctors will assess alcohol history, perform blood tests for nutritional deficiencies, and may request a brain scan to identify damage.
Early diagnosis is essential. The sooner alcohol use stops and thiamine levels are restored, the better the chances of stabilising or improving symptoms.
Can alcohol-related dementia be reversed?
Recovery depends on several factors:
- Duration and severity of alcohol use
- How early treatment begins
- Whether the person achieves complete abstinence
- Overall health and nutrition
Many people show significant improvement in memory, balance, and daily function within months of stopping drinking, particularly with appropriate medical and psychological support.
Treatment and recovery
Medical care
In the early stages, hospital treatment is often necessary. Doctors typically provide:
- Thiamine (vitamin B1) injections or tablets
- Fluids and electrolyte balance to restore hydration
- Medication to manage alcohol withdrawal safely
Withdrawal can cause agitation, hallucinations, or severe anxiety. Professional medical supervision is essential for safety.
Psychological and social support
Once physical health stabilises, long-term recovery focuses on therapy, counselling, and lifestyle changes. Support groups such as Alcoholics Anonymous (AA) help maintain abstinence and provide emotional connections.
Cognitive rehabilitation (structured activities that stimulate thinking and memory) can also support brain recovery.
Nutrition and lifestyle
A balanced diet rich in protein, fruits, and vegetables, combined with daily exercise and social contact, supports healing. Continued abstinence from alcohol remains the single most important factor in long-term recovery.
Caring for someone living with alcohol-related dementia
Supporting a family member through alcohol-related dementia can be demanding. Behavioural changes, denial, and mood swings often make caregiving difficult. These reactions are symptoms of brain damage, not deliberate choices.
Live-in care provides consistent support at home, making sure medication, meals, and daily routines are managed safely. This structured approach helps maintain independence while providing clinical oversight.
At Hometouch, our carers receive specialist training in dementia care. They provide structure, companionship, and practical support tailored to each person’s needs.
For guidance on whether live-in care might be suitable, read our comparison of live-in care vs care homes or speak to one of our care experts.
Supporting yourself as a carer
Watching a family member struggle with alcohol-related brain changes is difficult. Feelings of frustration or concern are normal responses to a challenging situation.
Counselling, peer support groups, and respite care can help you maintain your own wellbeing while continuing to provide support. Our clinical team has guided thousands of families through similar situations and can help you understand your options.
When to consider extra help
If your family member does any of the following, it may be time to consider structured, professional care.
- Struggles to eat, bathe, or take medication independently
- Becomes confused about their surroundings
- Shows unpredictable or unsafe behaviour
- Refuses medical advice or continues to drink
A live-in carer ensures safety, provides consistency, and reduces family stress. Alternatively, short-term respite care allows you time to plan next steps.
For more guidance on recognising care needs, read how to tell an elderly parent they need help.
Long-term outlook
With early intervention, proper nutrition, and complete abstinence, many people living with alcohol-related dementia can maintain independence or manage with minimal support. However, if damage is severe or drinking continues, cognitive decline may progress rapidly.
The most important priorities are safety, stability, and appropriate support. Structured care and healthy routines can significantly improve quality of life.
Facing alcohol-related dementia can be challenging, but recovery and stability are possible with the right help. Early action, medical support, and compassionate care can give your loved one the best chance of living with dignity and hope.
If you’re exploring care options, our friendly advisers can guide you through live-in care and home support tailored to your family’s needs. Speak to a Hometouch care adviser today to learn how we can help.