When caring for someone with dementia, you may notice their confusion and agitation increase as daylight fades. This common pattern, known as sundowning, affects many people living with dementia and can be particularly challenging for families.
Our clinical team regularly helps families navigate this specific aspect of dementia care. In this article, we’ll explain what causes sundowning, how to recognise it, and practical strategies to help manage these difficult evening hours.
If you’re starting to notice changes in your loved one’s mood or behaviour, our guide on how to tell an elderly parent they need help offers gentle ways to start the conversation.
What is sundowning?
Sundowning describes a pattern of increased confusion, agitation or anxiety that occurs in the late afternoon or early evening. It is “thought to affect approximately 20% of people with dementia, and around 80% of people with dementia in residential settings like care homes.”
People living with dementia may become restless, irritable, or emotionally distressed as light fades, with symptoms typically easing by morning.
Understanding why this happens can help you support your loved one through these challenging periods and reduce distressing episodes.
What causes sundowning in dementia?
While the exact cause isn’t fully understood, researchers believe a combination of biological and environmental factors may be involved.
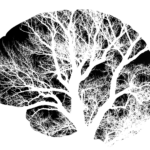
- Disrupted circadian rhythm – Dementia can affect the brain’s internal clock that regulates sleep, wakefulness, and mood. As natural light diminishes, this disruption can trigger confusion or agitation.
- Mental and physical exhaustion – By late afternoon, someone with dementia may have depleted their energy reserves. When communication is impaired, agitation becomes their way of expressing discomfort, thirst, or fatigue.
- Environmental factors – Poor lighting, background noise, unfamiliar routines, or overstimulation can all contribute to evening confusion.
- Sensory difficulties – Changes in vision or hearing can make environments feel more confusing as darkness approaches.
Recognising these triggers allows you to create calmer evenings and prevent distress before it escalates.
Recognising the signs of sundowning
Sundowning symptoms vary between individuals and often become more noticeable as dementia progresses. Episodes typically begin around sunset and may continue into the night, disrupting sleep for both the person with dementia and their family.
Common signs of sundowning include confusion, emotional outbursts, pacing, restlessness, paranoia, hallucinations, and disrupted sleep.
Specific symptoms include:
- Confusion or disorientation
- Increased agitation or emotional outbursts
- Pacing or wandering
- Restlessness or anxiety
- Paranoia, such as hiding possessions or mistrusting familiar people
- Hallucinations
- Difficulty sleeping or reversed sleep patterns
As dementia advances, sundowning symptoms may blend with other behavioural changes. Discuss any new or worsening symptoms with your GP or clinical care team so support can be adjusted appropriately.
When does sundowning occur in dementia?
Sundowning is most common in the middle to late stages of dementia. It affects people with all types of dementia – including Alzheimer’s disease, vascular dementia, frontotemporal dementia, and Lewy body dementia.
Once episodes begin, they may lengthen and interfere with normal sleep patterns, creating a cycle of fatigue and worsening confusion. While sundowning cannot be prevented entirely, symptoms can be managed through consistent routines, a calm environment, and professional support.
Professional live-in carers trained in dementia care can help establish patterns that reduce late-day stress and provide reassurance during difficult periods.
Can sundowning happen without dementia?
Yes. Although most common in people living with dementia, sundowning-like symptoms can occur in older adults without a dementia diagnosis. As the brain ages, its ability to regulate sleep and respond to stress weakens, leading to evening irritability, anxiety, or restlessness.
People with anxiety disorders may also experience evening agitation when their sleep-wake cycle becomes disrupted. Mental strain accumulated during the day can peak in the late afternoon, causing restlessness even in otherwise healthy adults.
If you notice these signs in someone without a dementia diagnosis, speak with their GP. Some reversible causes, including medication side effects, depression, or infections, can produce similar symptoms.
Managing sundowning: Practical strategies
While there’s no single treatment for sundowning, a structured and reassuring routine can significantly ease symptoms. Our clinical team recommends these approaches:
- Maintain consistent daily routines – Predictability reduces anxiety and helps your loved one feel more secure.
- Support healthy sleep patterns – Limit caffeine and daytime naps to encourage restful nighttime sleep.
- Encourage daytime activity – Gentle exercise and exposure to natural light help support the body’s circadian rhythm.
- Create a calm evening environment – Use soft, consistent lighting to prevent shadows and confusion. Reduce background noise and visual clutter.
- Provide reassurance and companionship – Your calm presence and gentle conversation help your loved one feel safe during periods of agitation.
- Use familiar music – Playing music they know and enjoy can soothe distress and provide comfort.
If these episodes become unpredictable or unsafe, a professional dementia carer can help defuse tense situations and support daily routines safely at home. If symptoms worsen or significantly disrupt daily life, discuss medication options with your GP. Low-dose melatonin or other medications may help in some cases, but should only be used following a professional assessment.
For additional guidance on managing challenging behaviours, read our article on aggressive behaviour in dementia.
Supporting your loved one through sundowning
Sundowning can be distressing for both the person with dementia and their family, but understanding its causes and recognising the signs allows you to respond with confidence. By establishing calm routines and creating a reassuring environment, you can help reduce the frequency and intensity of these difficult episodes.
If you need additional support managing sundowning or other aspects of dementia care, our clinical team is here to provide guidance tailored to your family’s situation.